oral tumors
BACKGROUND
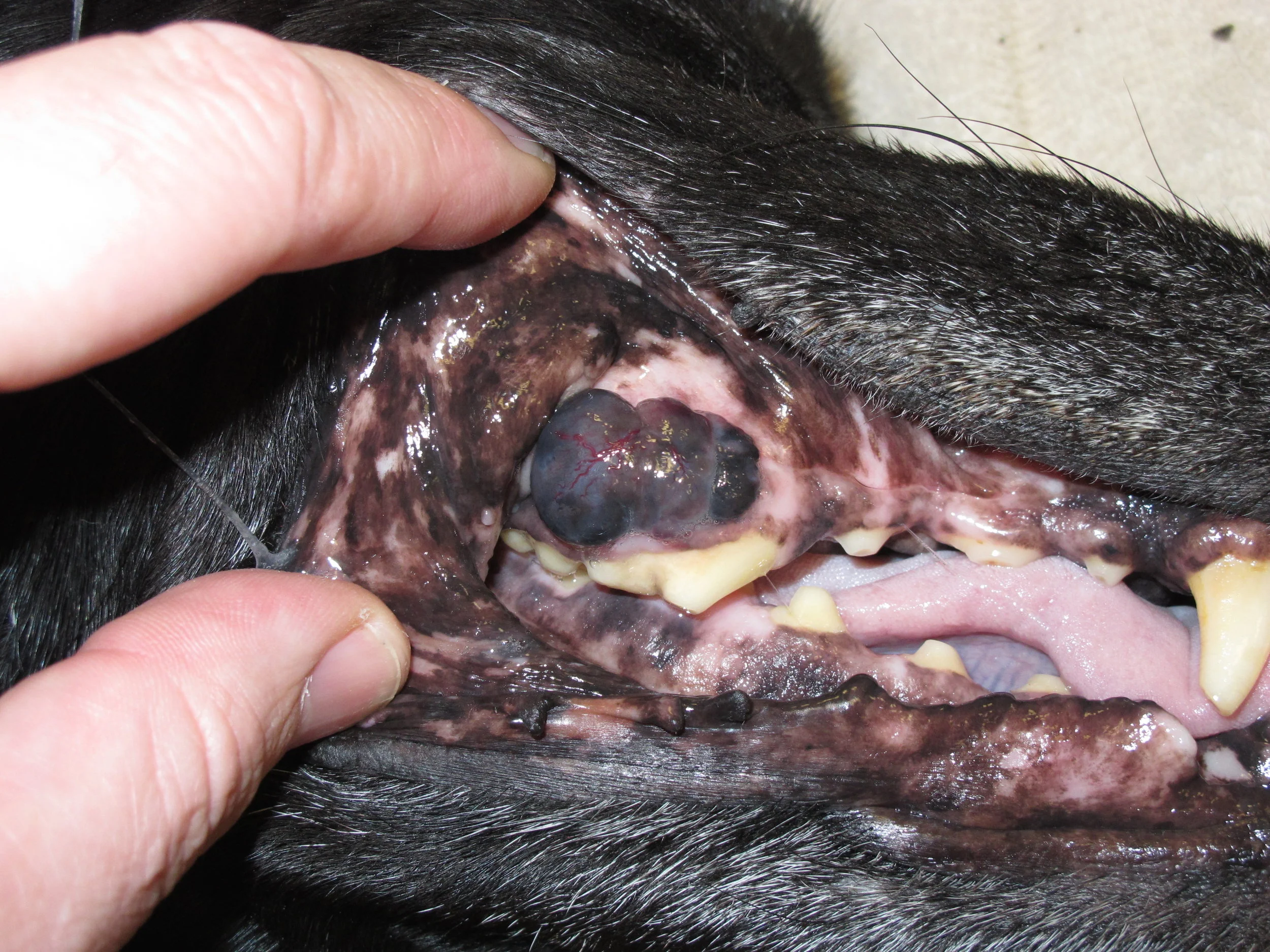
Oral tumors are relatively common in cats and dogs and can occur in the mandible (lower jaw), maxilla (upper jaw), palate, tongue, tonsils, and pharynx. Squamous cell carcinoma (SCC) is the most common oral tumor in cats, while the remaining 10% of feline oral tumors include malignant (fibrosarcoma, osteosarcoma, salivary gland carcinoma, lymphoma, malignant melanoma, and chondrosarcoma) and benign tumors (acanthomatous ameloblastoma, osteoma, and inductive fibroameloblastoma). Malignant melanoma and SCC are the most common oral tumors in dogs, but others include benign (peripheral odontogenic fibroma and acanthomatous ameloblastoma) and malignant tumors (fibrosarcoma, osteosarcoma, and multilobular osteochondrosarcoma). Malignant melanoma is associated with a high risk of metastasis, but the majority of other malignant tumors in cats and dogs have a low rate of metastasis.
DIAGNOSIS
Oral tumors are diagnosed by a combination of visual examination, incisional biopsy, and either radiographs or CT scan. Fine-needle aspirates are usually non-diagnostic because of the degree of inflammation and necrosis commonly encountered with oral tumors. Radiographs or, preferably, CT scan are recommended to determine the location and extent of the oral tumor and surgical planning.
CLINICAL STAGING
The two most common sites of metastasis for oral tumors are the regional lymph nodes and lungs. There are three major pairs of lymph nodes in the head and neck region (mandibular, medial retropharyngeal, and parotid lymph nodes) as well as minor lymph nodes (such as the buccal or facial lymph nodes). However, only the mandibular lymph node is palpable. In addition, the lymphatic drainage pattern of oral tumors is unpredictable and can drain into any of these lymph nodes as well as contralateral lymph nodes. In one study of 31 cats and dogs with metastatic oral tumors, metastasis was reported to the mandibular lymph node in 55% of animals and to the medial retropharyngeal and parotid lymph nodes in the remaining 45% of animals. Surgical techniques have been described to harvest the mandibular, medial retropharyngeal, and parotid lymph nodes from one side of the head and neck, and both the left and right mandibular and medial retropharyngeal lymph nodes from a single approach; however, both have the potential to miss metastatic lymph nodes and are associated with a more extensive surgical approach with presumably an increased risk of complications. For this reason, sentinel lymph node mapping and biopsy are recommended. This involves peritumoral injection of a lipid-soluble contrast agent 24 hours prior to surgery (usually under sedation), regional radiographs or CT scan immediately prior to surgery to identify the sentinel lymph node, and then peritumoral blue dye injection during surgery to aide in intraoperative identification and excision of the sentinel lymph node.
Thoracic CT scans, particularly if a CT scan is being performed for evaluation of the oral tumor, or radiographs are recommended for assessment of metastasis to the lungs.
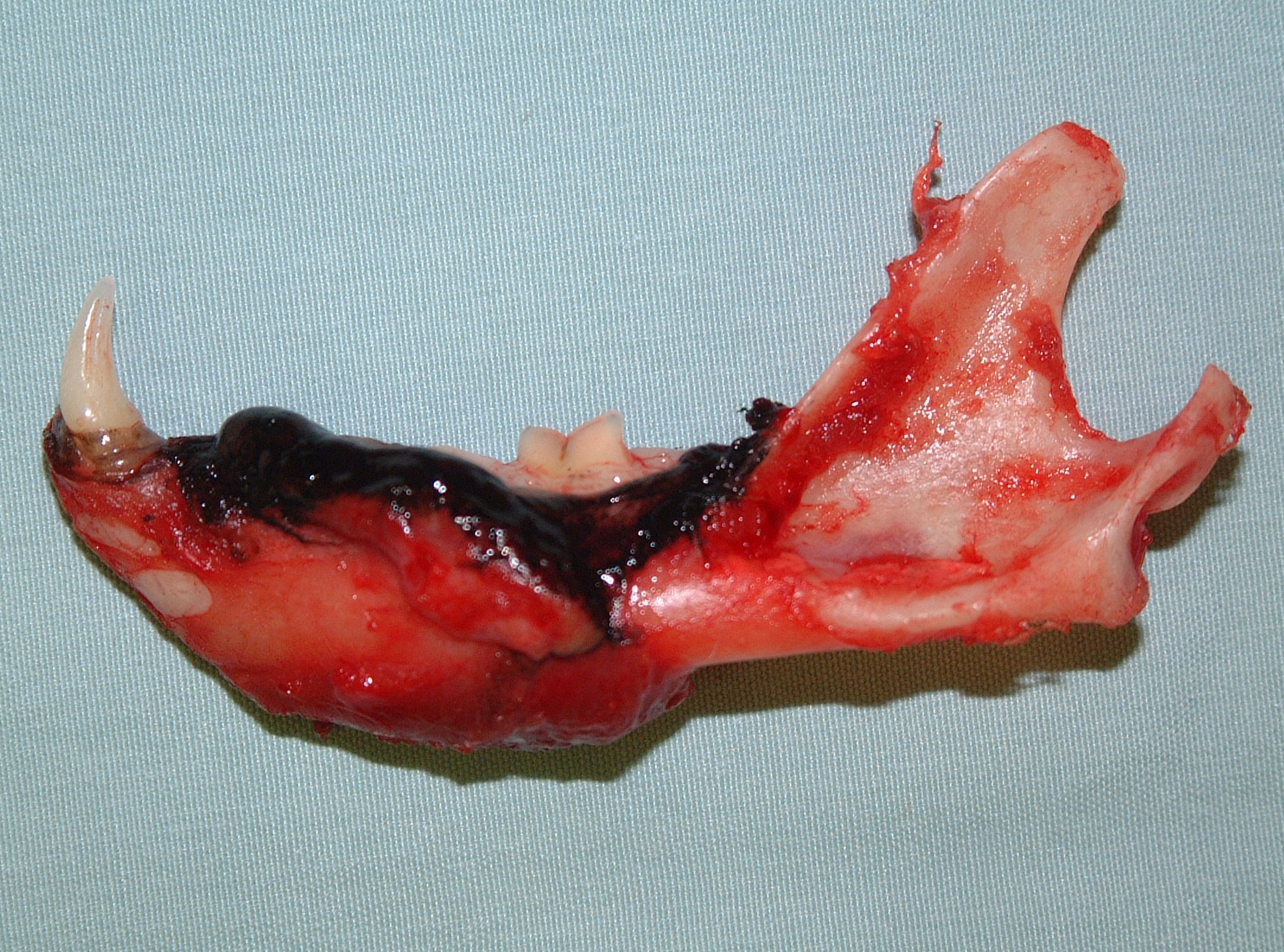
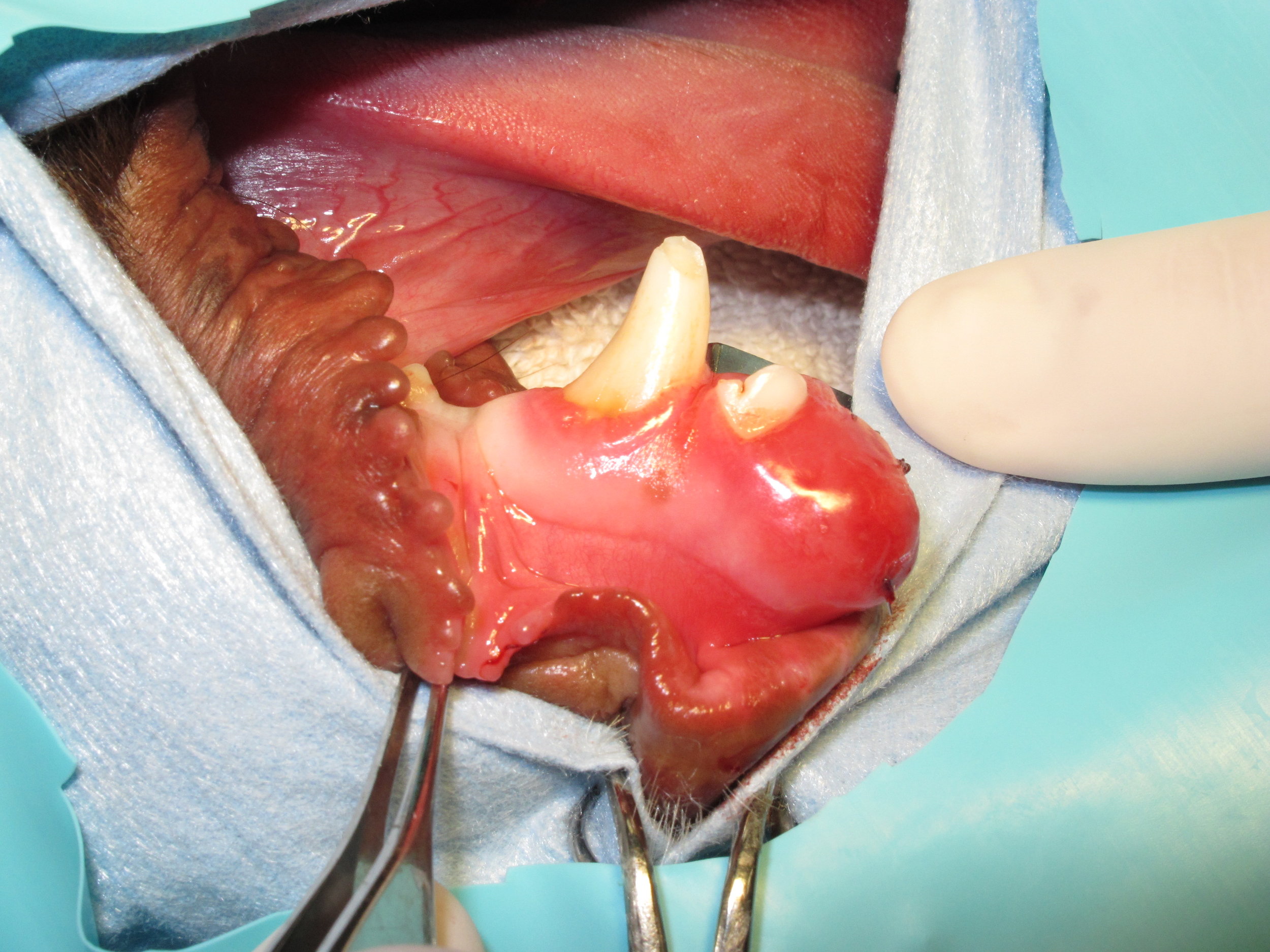
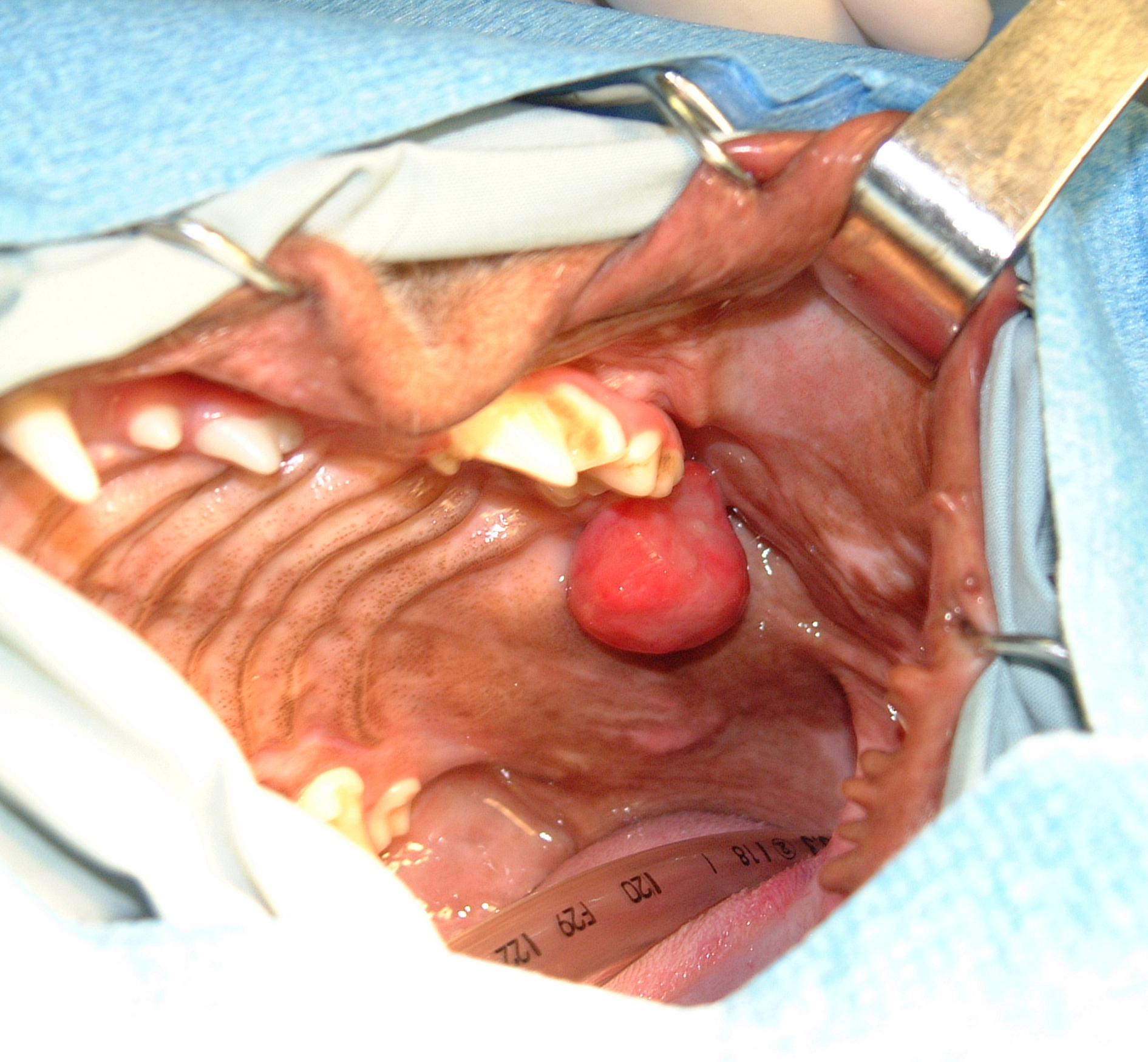
TREATMENT
Surgical resection is the recommended treatment for all oral tumors.. Other than benign peripheral odontogenic fibromas, surgical resection of all other oral tumors involves removal of bone. These procedures are called mandibulectomy (for removal of part of the lower jaw) and maxillectomy (for removal of part of the upper jaw). The function and cosmetic appearance of dogs (ie, eating, drinking and playing) following mandibulectomy is usually very good to excellent with a return to voluntary eating in 44% of dogs by day 1, 70% of dogs by 2, 90% of dogs by day 3, and 97% of dogs by day 4 after surgery. In contrast, a feeding tube is recommended in cats as up to 72% of cats will have immediate eating difficulties and 12% of cats will never eat again following mandibulectomy. The functional performance and cosmetic appearance after maxillectomy is usually very good to excellent in both cats and dogs, and feeding tubes are rarely required following maxillectomy in cats, but this can depend on the location of the tumor and extent of the surgery.
Custom computer-designed and 3D-printed mandibular prostheses have been used in one cat and a small series of dogs for reconstruction following mandibulectomy. Reconstruction of mandibular defects may minimize the risk of complications resulting from surgical resection of portions of the mandible and result in better functional results, particularly in cats.
For images of postoperative appearance following the different types of mandibulectomy and maxillectomy procedures, please select the appropriate link below:
Immunotherapy (tumor vaccine) is recommended for dogs with malignant melanoma because of the high risk of metastasis to the lymph nodes and lungs. Chemotherapy is recommended for dogs with oral osteosarcoma. Chemotherapy should also be considered for other oral tumors and the palliative management of cats with SCC.
PROGNOSIS
Dogs
Malignant Melanoma
Malignant melenoma is the most common oral tumor in dogs and also has the highest metastatic potential, particularly to the regional lymph nodes and lungs. Based on a combination of early papers, the local recurrence rate following mandibulectomy was 22% with a median survival time of 9-11 months and a 1-year survival rate of 21%. Similarly, the local recurrence rate following maxillectomy is as high as 48% with a median survival time of 5-10 months and a 1-year survival rate of 27%. However, in two large 2014 studies, the overall local recurrence rate was 16%-17%. Clinical stage has prognostic significance with median survival times of 20 months for dogs with stage I disease, (non-metastatic melanoma < 2cm), 5-20 months for dogs with stage II disease (non-metastatic melanoma between 2cm-4cm), 3-6 months for dogs with stage III (non-metastatic melanoma > 4cm or melanoma with lymph node metastasis), and up to 6 months for dogs with stage IV disease (melanoma with distant metastasis). However, in a more recent 2014 paper, the median progression-free interval and median survival time were 508 days and 723 days for dogs with stage I-III disease treated with either mandibulectomy or maxillectomy, respectively. Prognostic factors in this study included local tumor size (with median survival times of 874 days for tumors < 3cm and 376 days for tumors > 3cm, respectively) and clinical stage (with median survival times of 874 days, 818 days, and 207 days for dogs with stage I, II, and III disease, respectively).
Oral melanoma is also responsive to radiation therapy, particularly coarse radiation protocols. The overall response rate varies from 83%-94% with a complete response rate as high as 70%. For dogs with a complete response, the local recurrence rate is 15%-26% with a median time to local recurrence of 139-235 days. The metastatic rate is 51%-58% with a median time to metastasis of 311 days. The median survival time varies from 210-363 days with 1- and 2-year survival rates of 23%-48% and 21%, respectively. Survival times are significantly improved with rostrally located melanomas, melanomas with no radiographic evidence of bone lysis, and incompletely excised melanomas with no evidence of gross disease. In a 2015 study, the median survival times were 758 days, 278 days, 163 days, and 80 days for dogs with stage I, II, III, and IV oral melanoma treated with radiation therapy, respectively.
Overall, the median survival times for dogs with oral malignant melanoma are 65 days with no treatment, 240-874 days with surgical resection, and 210-363 days with radiation therapy, with most dogs dying as a result of metastatic disease. Numerous recent studies have shown that postoperative chemotherapy does not provide a survival benefit. While controversial in some retrospective papers, immunotherapy (ie, melanoma vaccine) has significantly improved the outcome of dogs with all stages of oral malignant melanoma. In one prospective study published in 2011, 58 dogs with locoregional control of their oral malignant melanoma and adjunctive treatment with a vaccine containing plasmid DNA with an insert encoded for human tyrosinase were compared to a historical control of 53 dogs with locoregional control of their oral melanoma. Regardless of clinical stage, 26% of dogs treated with the melanoma vaccine died as a result of their oral melanoma compared to 64% of dogs in the historical control group. The overall median survival time was significantly longer for dogs in the vaccination group (not reached because > 50% of dogs were cured) compared to the median survival time of 324 days in the historical control group. The median survival times for dogs with stage II (324 days) and stage III (338 days) were not significantly different in the historical control group; however, there was a significant difference between clinical stages in the vaccination group with a median survival time not reached for dogs with stage II disease compared to a median survival time of 235 days in dogs with stage III oral melanoma. The most likely explanation for this is that a humoral response to the melanoma vaccine is detected 3-9 months after completion of the melanoma vaccine protocol and dogs may not develop an effective immune response prior to the development of metastatic disease with more aggressive oral melanomas.
A second melanoma vaccine has been developed using electrovaccination of human chondroitin sulphate proteoglycan-4 (CSPG4). The 1- and 2-year survival rates for dogs with stage II and III oral melanoma treated with surgery alone were 63% and 5%, respectively, but 96% and 30%, respectively, for dogs treated with surgery and the CSPG4 vaccine. Furthermore, 39% of dogs developed metastatic disease after being treated with the adjuvant CSPG4 vaccine compared to 79% in dogs treated with surgery alone.
Squamous Cell Carcinoma
Squamous cell carcinoma, depending on the paper, is either the most common or second most common oral tumor in dogs. The local recurrence rate following either mandibulectomy or maxillectomy is <10%, metastasis to the regional lymph nodes occurs in <10% of dogs and to the lungs in 3%-36% of dogs. The median survival time for untreated dogs is 54 days with a 0% 1-year survival rate. Following mandibulectomy, local tumor recurrence is reported in 0%-10% of dogs. Median survival times for dogs with mandibular SCC treated with surgery alone varies from 19-43 months with 1-, 2-, and 3-year survival rates of 88%-100%, 79%, and 58%, respectively. Median survival times for dogs with maxillary SCC treated with maxillectomy varies from 10-39 months with 1-, 2-, and 3-year survival rates of 57%-94%, 69%, and 38%, respectively. Clinical stage was prognostic in a 2013 clinical study with median survival times not reached (and 94% 1-year survival rate), 420 days, 365 days, and 50 days for dogs with stage I, II, III, and IV oral SCC, respectively. A histologic risk score was developed in this study based on tumor-associated inflammation, lymphatic or vascular invasion, and invasion of peripheral nerves. Dogs with a risk score of two or greater had a significantly worse prognosis with a median survival time of 365 days and a 1-year survival rate of 36% compared to a median survival time which was not reached and an 80% 1-year survival rate for dogs with a risk score of 0 or 1.
Fibrosarcoma
Fibrosarcoma is the third most common oral tumor in dogs. Metastasis to the regional lymph nodes and lungs is reported in 19%-22% and up to 27% of dogs, respectively. While surgery is the recommended treatment for dogs with oral fibrosarcoma, there may also be a role for radiation therapy because of previous reports of high local recurrence rates (up to 59%) following either mandibulectomy or maxillectomy. However, this has not been confirmed and the local tumor recurrence rates are much lower in more recently published studies. In a 2012 study, the local recurrence rate in 29 dogs with oral fibrosarcoma treated with either mandibulectomy or maxillectomy was 24%, while the metastatic rate was 24%, the median survival time was 743 days, and the 1- and 2-year survival rates were 88% and 58%, respectively.
Osteosarcoma
Mandibular osteosarcoma has traditionally been considered a less aggressive and more curable disease than osteosarcoma of the appendicular skeleton. Reported local recurrence rates are 4%-18%, metastatic rates are 29%-58%, and 1-year survival rates of 35%-71%. In a 2015 paper on 50 dogs with mandibular osteosarcoma, the local recurrence rate was 18%, the metastatic rate was 58%, and the overall median survival time of 525 days with a 1-year survival rate of 50%. Prognostic factors included mitotic index, histologic grade, and treatment with chemotherapy. The median survival times for dogs with a mitotic index of less than or equal to and greater than 40 per 10 high power fields were 637 days and 256 days, respectively. The median survival times for dogs with grade I and grade II/III mandibular osteosarcomas were 648 days and 306 days, respectively; the 1-year survival rates were 77% for dogs with grade I and 24% for dogs with grade II/III mandibular osteosarcoma; and dogs with grade II/III osteosarcomas had a 2.8-times greater hazard of tumor-related death than dogs with grade I mandibular osteosarcoma. The median survival times for dogs treated with surgery alone and surgery and chemotherapy were 525 days and 1023 days, respectively; and dogs not treated with chemotherapy had a 2.8-times greater hazard of tumor-related death than dogs treated with mandibulectomy and chemotherapy.
There is a paucity of information on the outcome for dogs with maxillary osteosarcoma and most of this information is based on studies published in the 1990s. In these studies, which were published before the common use of CT scans for surgical planning and improved anesthetic, surgical, and postoperative management techniques, median survival times of 30 months, 8 months, and 5 months were reported for dogs with osteosarcoma of the rostral, central, and caudal maxilla, respectively.
Cats
Squamous Cell Carcinoma
The prognosis is guarded for cats with oral SCC. This is a frustrating disease to manage and treat because the tumor is often quite large, extensive, and invasive, especially relative to the small size of the oral cavity in cats. Many different treatment options and combinations have been investigated including surgery, radiation therapy, and chemotherapy. The most challenging problem in cats with oral SCC is prevention of the local tumor from either recurring or progressing. In one study of 49 cats with oral SCC, 84% of cats died because of either recurrence or progression of their tumor. Because of the high rate of failure to control the local tumor, there is a paucity of information on the long-term risk of metastasis. In one study, metastasis was reported to the regional lymph nodes and lungs in 31% and 10% of cats, respectively.
In one study of 21 cats with SCC treated with mandibulectomy alone, the local recurrence rate was 38%, the median survival time was 217 days, and the 1- and 2-year survival rates were 43% and 43%, respectively. Tumor location and extent of surgery were prognostic in this study with median survival times of 911 days for rostral tumors, 217 days for cats treated with hemimandibulectomy, and 192 days when > 50% of the mandible was resected. In an older study of seven cats treated with mandibulectomy and radiation therapy, the median survival time was 14 months with a 1-year survival rate of 57%, although local tumor recurrence was reported in 86% of cats between 3-36 months after surgery. Many other treatments have been investigated for cats with oral SCC. The median survival time for cats treated with palliative radiation therapy is 113-175 days. Prognostic factors include tumor location (median survival time for sublingual SCC is 135 days which is significantly longer than the median survival time of 80 days for mandibular SCC) and tumor size (with significantly better outcomes for SCC < 2cm).
Fibrosarcoma
Six cats with mandibular fibrosarcoma were reported in one series of cats treated with mandibulectomy. Two cats developed local tumor recurrence prior to 1 year and the remaining cats were disease-free at both 1- and 2-years resulting in a 2-year survival rates of 67%.
Osteosarcoma
Six cats with mandibular osteosarcoma were reported in one series of cats treated with mandibulectomy. One cat developed local tumor recurrence prior to 1 year and the remaining cats were disease-free at both 1- and 2-years resulting in a 2-year survival rates of 83%.
Last updated on 6th March 2017