SEGMENTAL AND RIM MANDIBULECTOMY
Segmental mandibulectomy is a surgical procedure involving removal of a segment of the mid-body of the mandible while preserving both the rostral and caudal mandible. This technique is indicated for benign oral tumors, such as acanthomatous ameloblastoma and either small or low-grade malignant tumors, of the mid-mandibular ramus. The overall complication rate following segmental mandibulectomy in dogs is 33%, including dehiscence and mandibular drift with associated malocclusion.
Rim mandibulectomy is similar to a segmental mandibulectomy in terms of indications and technique; however, the ventral cortex of the mandibular ramus is preserved with a cresenteric osteotomy. Preservation of the ventral cortex of the mandible prevents mandibular drift and malocclusion associated with segmental mandibulectomy.
The overall complication rate following segmental mandibulectomy in dogs is 33%. The most common complications are wound dehiscence (17%) and short-term eating difficulties (up to 44% overall with 30%, 70%, 90%, and 97% of dogs returning to voluntary eating by day 1, 2, 3, and 4, respectively).
Complications are more frequently encountered in cats with 67% of cats having both short- and long-term complications. The most common complications are eating difficulties and/or dysphagia. Mandibular drift, with subsequent malocclusion and trauma to the overlying hard palate, is reported in 67% of cats following segmental mandibulectomy. Grooming difficulties and tongue protrusion are also common. Despite this high complication rate and need for supplemental nutrition via a feeding tube postoperatively, 83% of owners were satisfied with the outcome following mandibulectomy in their cats.
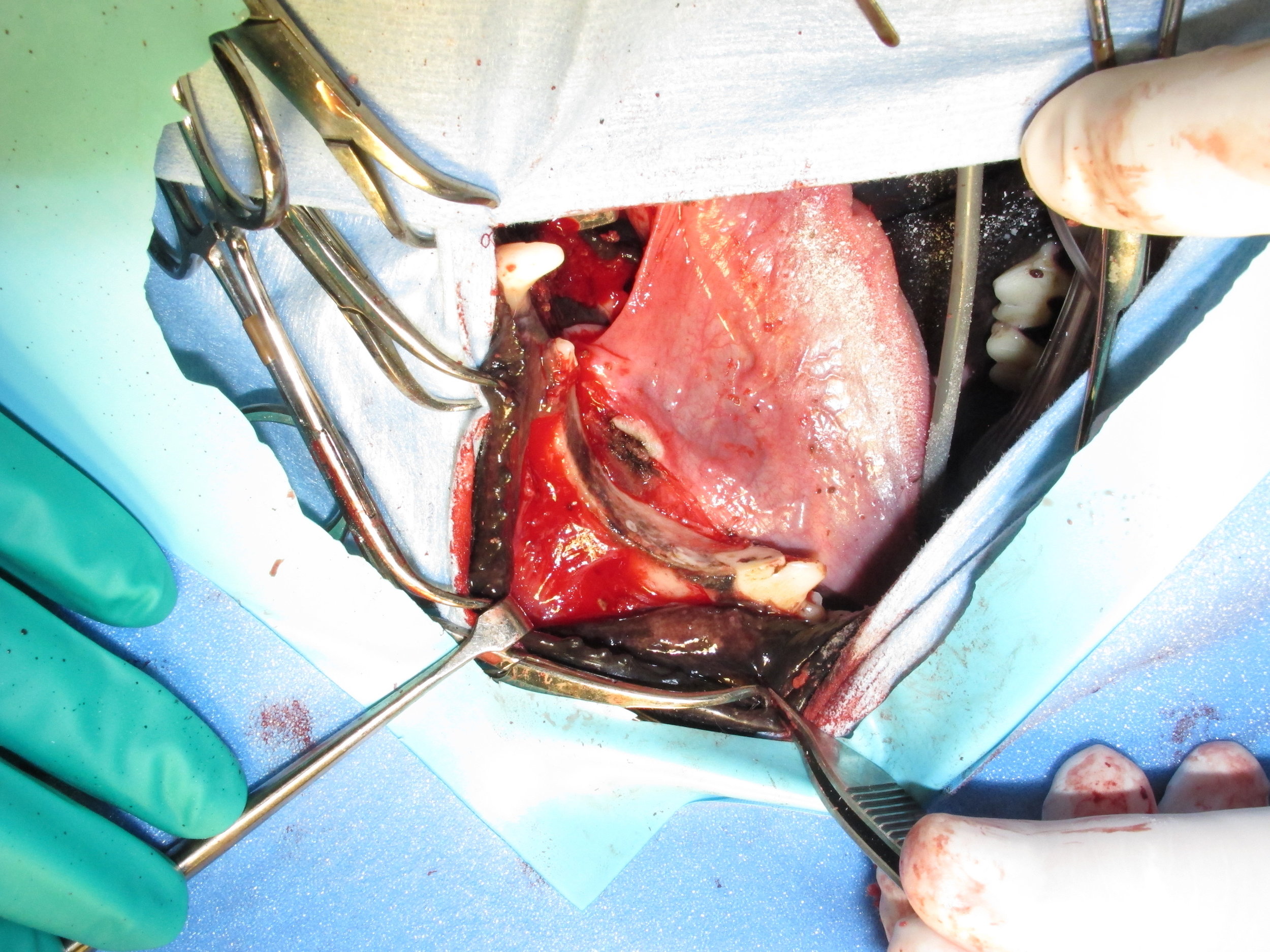
Case 1 - Segmental Mandibulectomy for an Acanthomatous Ameloblastoma
Case 2 - Segmental Mandibulectomy for a Fibrosarcoma
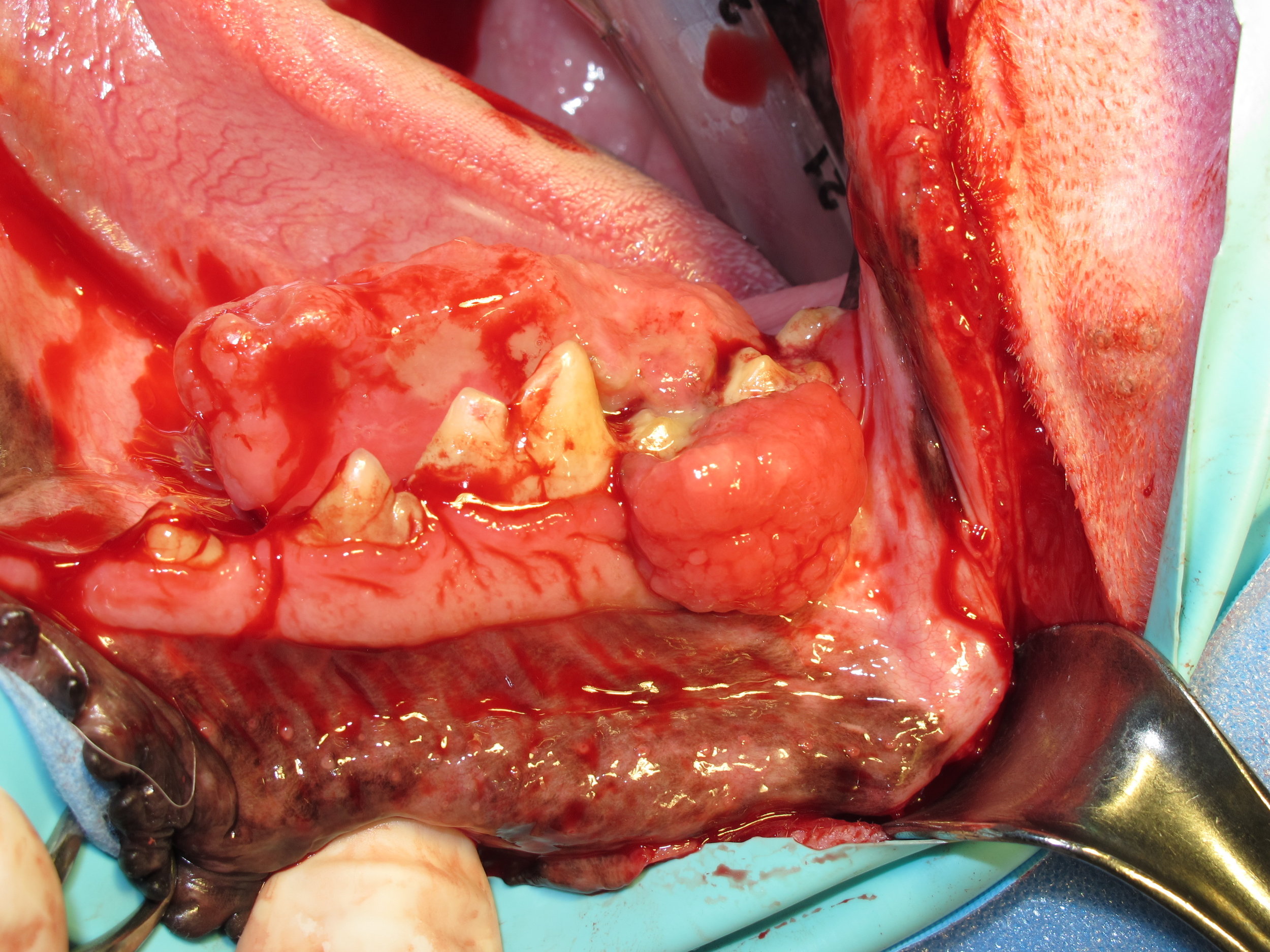
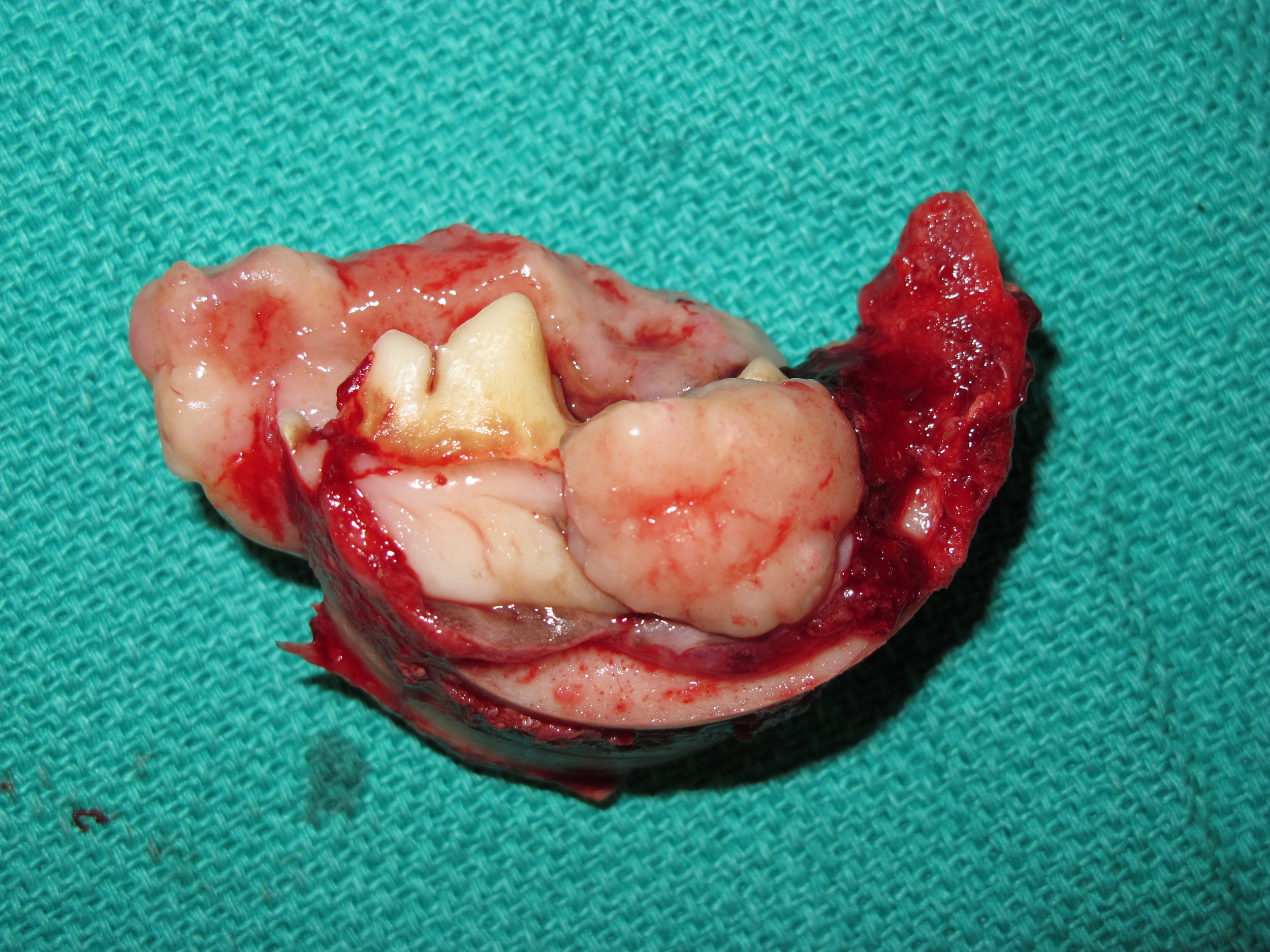
Case 3 - Rim Mandibulectomy for a Recurrent Peripheral Odontogenic Fibroma
Case 4 - Rim Mandibulectomy for a Recurrent Peripheral Odontogenic Fibroma
Last updated on 6th March 2017