Orbitectomy for a Dog with a Grade I Multilobular Osteochondrosarcoma
Signalment: 3.5-year-old, FS, golden retriever
History:
This dog was referred after a 2-month history of right-sided conjunctivitis and increased intraocular pressure (21-25 mm Hg) progressing to exophthalmos with an inability to retropulse the right eye. A CT scan was performed which showed a well-circumscribed osseous mass arising from the medial orbital bone.
Physical exam findings:
Mild to moderate right-sided exophthalmos
Inability to retropulse right eye
Diagnostic and clinical staging tests:
CBC: no abnormalities
Serum biochemistry: no abnormalities
CT scan: 3.2 cm x 3.4 cm x 3.9 cm osseous mass arising from the medial aspect of the right orbit, with mild enlargement of the right medial retropharyngeal lymph node. No evidence of lung metastasis.
Treatment:
Orbitectomy combined with resection of the zygomatic arch and coronoid process of the mandible.
Outcome:
Grade I multilobular osteochondrosarcoma (MLO) with complete excision (bone margins: 20.0 mm to 30.0 mm; deep margins: 11.0 mm)
Complications:
Blindness (OD), immediate. This was expected to some degree because of prolonged retraction on the optic nerve and vessels to expose the bone margins for resection of the mass.
Sneezing and difficulty opening jaw, 6 weeks postop. The cause for these remain undiagnosed and unresolved. While local tumor recurrence is a possibility, I think this is highly unlikely considering that this tumor was completely excised with very good surgical and histologic margins, and that this is a grade I MLO (which are typically slow growing tumors). A repeat CT has been recommended but this has not been done yet.
Video link: https://www.youtube.com/watch?v=eBrdiKihhZA&t=370s
Tags: #MLO #orbitectomy
Preoperative CT scan showing a large osseous mass arising from the medial aspect of the right orbit.
Preoperative CT scan showing a large osseous mass arising from the medial aspect of the right orbit. Note that this mass extends to the orbital bone overlying the frontal lobe of the brain.
3D reconstruction showing the large orbital mass. These reconstructions are very helpful in surgical planning, especially the approach (in this case, zygomatic arch resection and resection of the coronoid process of the mandible) and the margins (in this case, knowing that we would see brain and hence use a more delicate instrument to make the osteotomies in this region).
The initial surgical approach involved a skin incision along the zygomatic arch and extending on to the dorsolateral aspect of the caudal muzzle.
Electrosurgery was used to incise and elevate the temporal (pictured) and masseter muscles from the dorsal and ventral aspects of the zygomatic arch, respectively.
Soft tissues attached to the medial aspect of the zygomatic arch were freed using a periosteal elevator.
The first step to exposing the orbit is a zygomatic arch resection. Once the zygomatic arch is exposed and freed of all its soft tissue attachments, the caudal zygomatic bone osteotomy was performed with a sagittal saw. The periosteal elevator is positioned to protect the deeper soft tissues from iatrogenic trauma from the saw blade.
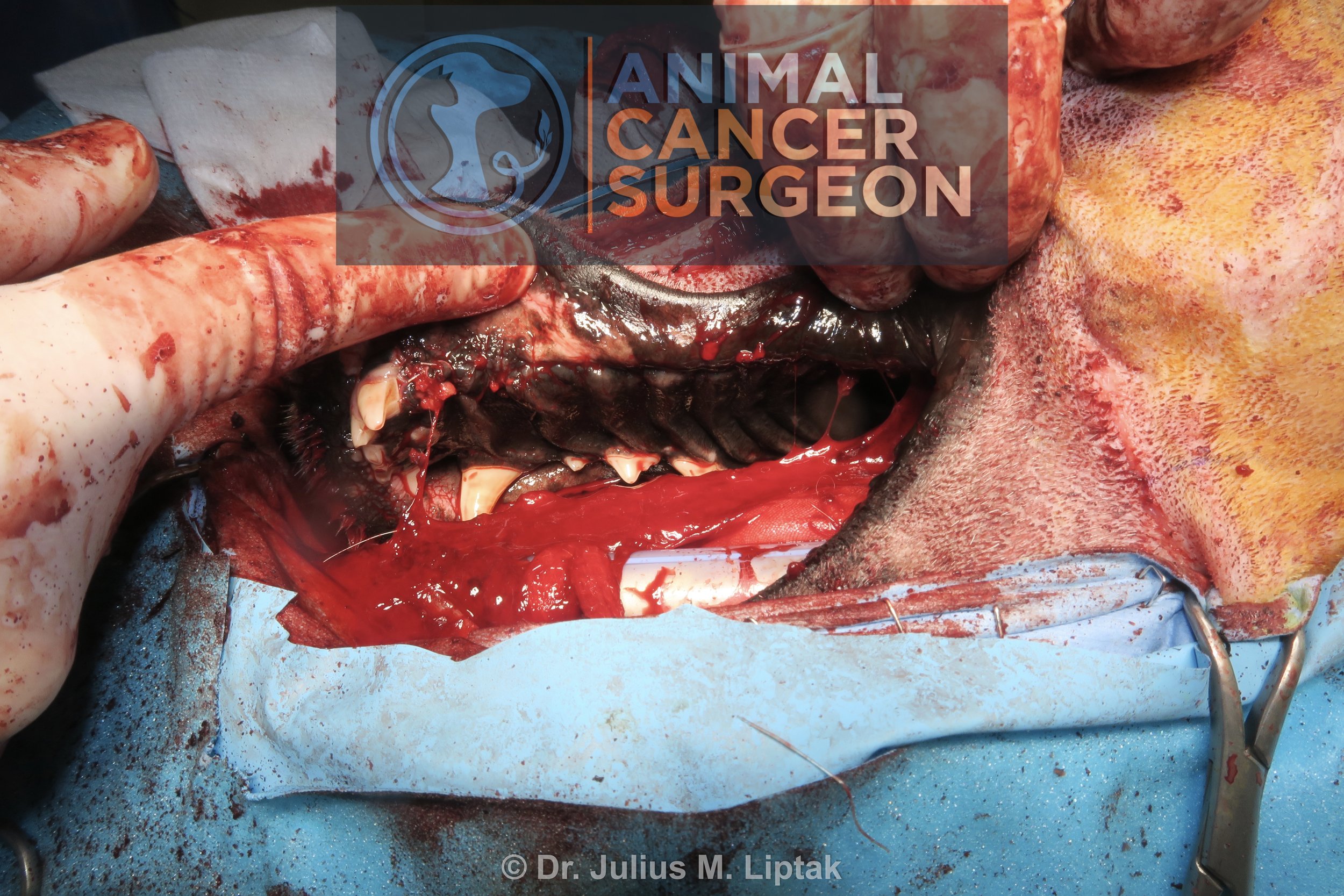
The rostral zygomatic arch resection was completed with a sagittal saw and osteotome and mallet. This osteotomy was done in such a way that a portion of the caudal maxilla was included in the osteotomy, but dorsal to the teeth.
The completed zygomatic arch resection before removal of the zygomatic arch. I do not replace the zygomatic arch after surgery. There is no functional need for it and I very rarely see a cosmetic defect as a result of its absence.
The orbit mass was easily exposed after dissecting through the superficial soft tissues; however, the caudal aspect of the mass and caudal orbit were difficult to visualize because of the vertical ramus of the mandible.
The coronoid process of the mandible was osteotomized with a sagittal saw dorsal to the temporomandibular joint to improve visualization of the caudal orbit.
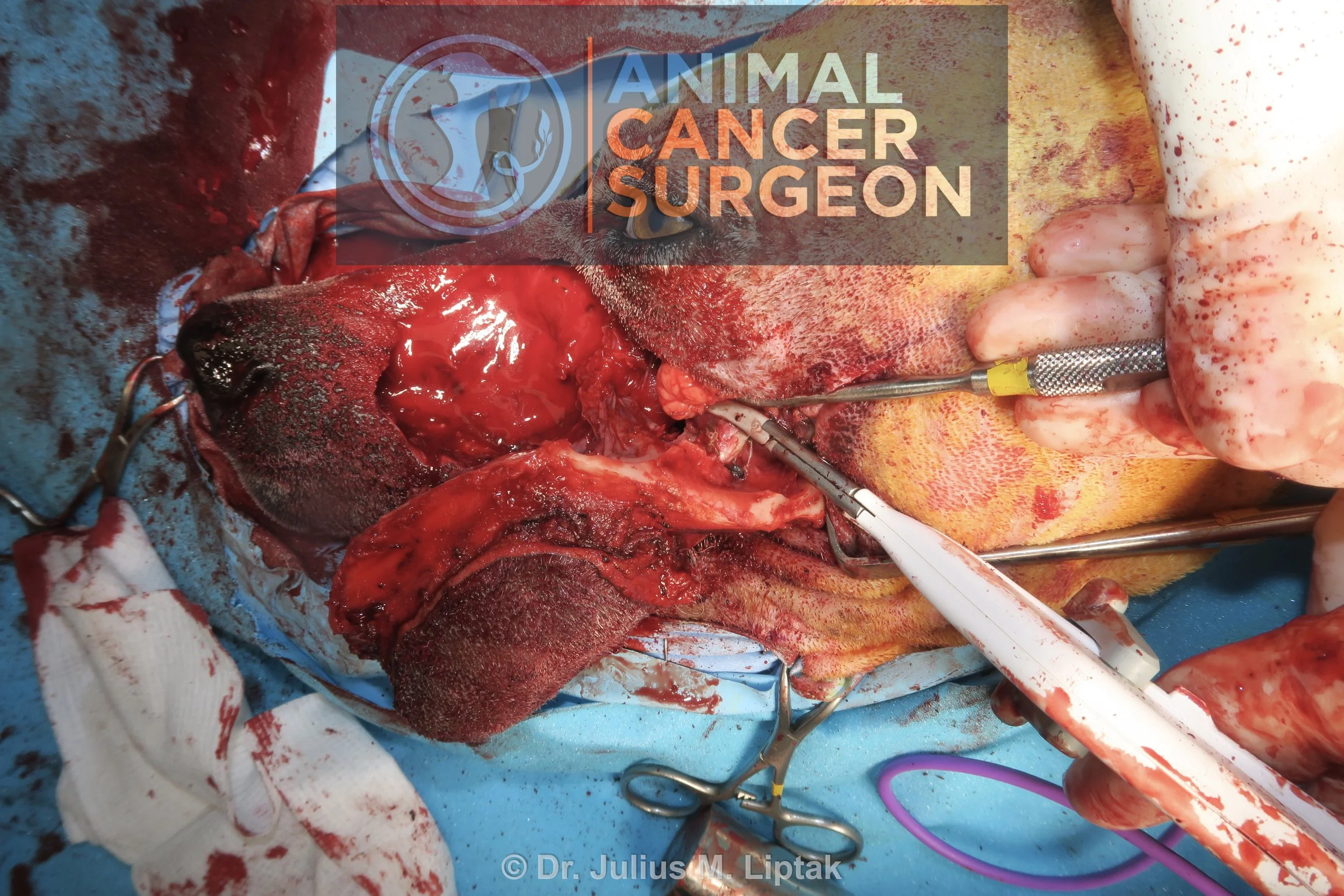
Following the removal of the coronoid process of the mandible, the exposure of the caudal orbit was markedly improved.
I wanted to save the eye, which we did anatomically, but the dog was blind in this eye after surgery. I suspect this was a result of protracted and marked retraction of the caudal globe structures (vessels and optic nerve) during resection of the mass. The majority of the dorsal osteotomy was done with a piezotome in an effort to reduce iatrogenic trauma to the underlying brain; however, while accurate and precise, a peizotome is a painfully slow technique to do osteotomies, even in thin bone such is in this region.
Intraoperative image of the orbitectomy site following removal of the orbital mass from the surgical field.
Bleeding from the meninges was controlled with hemostatic foam.
The wound was then closed primarily in three layers: temporal and masseter muscle fascia, subcutaneous, and skin.
Postoperative specimen image of the resected orbital mass. The mass had a small attachment to the orbital bone, which meant that bone margins were easier to achieve than if this had a broad-based attachment to the bone. Additional caudal margins were obtained because I was not satisfied with my original margins. Histologically, this was a complete excision with the narrowest histologically tumor-free margins being 11 mm.
Immediate postoperative CT scan showing the extent of the orbitectomy along the rostral aspect of the surgical field.
Immediate postoperative CT scan showing the extent of the orbitectomy along the caudal aspect of the surgical field at the level of the frontal lobe of the brain.
Reconstructed CT view of the orbitectomy.
Day 1 postoperative appearance. This swelling and bruising took over 1 week to subside. The swelling made initial assessment of eyesight difficult, but the dog did not have a menace reflex initially and had not regained a menace reflex by week 6 after surgery.