Signalment: 15.5-year-old, FS domestic shorthair cat
History:
This cat presented to her family veterinarian with a mandibular mass, and was then referred to a local specialty hospital. She had a previous history of small T-cell intestinal lymphoma, chronic pancreatitis, and progressive azotemia. Her small T-cell intestinal lymphoma was previously treated with chlorambucil and prednisolone but the chlorambucil was discontinued 9 months prior to the development of her oral mass. Fine-needle aspirate cytology of the mandibular mass was consistent with an osteosarcoma, which carries a very good prognosis in cats following surgery alone. She was initially treated with Palladia and one fraction of palliative radiation before the owner contacted me regarding the possibility of mandibulectomy and reconstruction with a patient-specific, 3D printed implant.
A CT scan was done at the local specialty hospital which showed a non-metastatic left mandibular mass. Resection was definitely possible based on this CT scan but the amount of bone stock available on the caudal left mandible was limited, making reconstruction with a patient-specific, 3D printed implant challenging. I worked with Laurent Lacombe at NXMed (https://nxmed.ca/home) to design a composite implant that would meet the challenging needs to reconstruct this defect, including a biocompatible PEKK implant to reconstruct the mandible, with the rostral mandible shortened by 15 mm, and a titanium plate to fix to the PEKK implant and residual mandibular bone.
Physical exam findings:
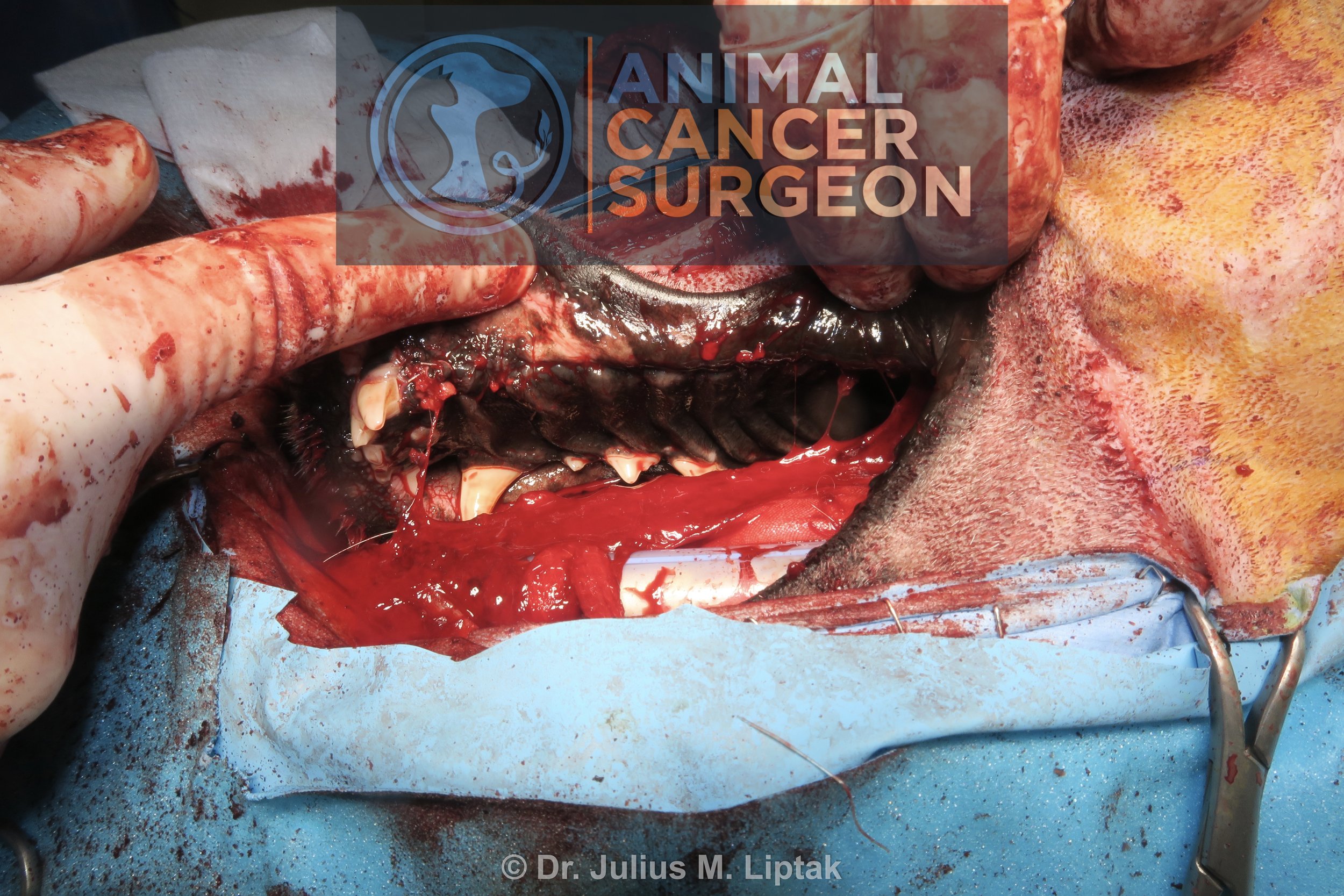
The cat was referred from New Jersey and presented to me at Capital City Specialty & Emergency Animal Hospital after the patient-specific implant had been manufactured and delivered to me, about 3 weeks after her CT scan. On examination, she had a large left mandibular mass extending to the rostral midline and caudally along the left mandible., much further caudally than on her CT scan. Unfortunately, her tumor had grown in the period between her CT scan and surgery, much more so than anticipated (as I had added an additional 1 cm to the caudal margins to account for this potential growth). I discussed the possibility of not being able to reconstruct her mandible with her owner and her owner decided to proceed with surgery with the plans of reconstructing if possible, modifying the reconstruction if different to the original plan pending the amount of available bone remaining, or proceeding with a radical mandibulectomy if reconstruction was not possible because of the caudal growth of the tumor along the left mandible.
Diagnostic and clinical staging tests:
Fine-needle aspirate: osteosarcoma
CBC: moderate anemia (PCV 24.5%) with mild leukocytosis and neutrophilia
Serum biochemistry: increased BUN (15.5 mmol/L) with high normal creatinine (137 umol/L)
Abdominal ultrasound: borderline increases in the size of the right kidney and pancreas
CT scan: left mandibular mass and no evidence of pulmonary metastasis
Three-view thoracic radiographs (immediately prior to surgery): no evidence of lung metastasis but a moderate diffuse interstitial pattern and cardiomegaly (cat had a grade III/VI heart murmur). Possibilities suggested for this interstitial pattern included pulmonary edema secondary to left-sided heart failure (unlikely because of she had no respiratory distress), an infiltrative neoplastic process such as lymphoma, or, less likely, pulmonary hemorrhage, pulmonary fibrosis, or interstitial pneumonia.
Treatment:
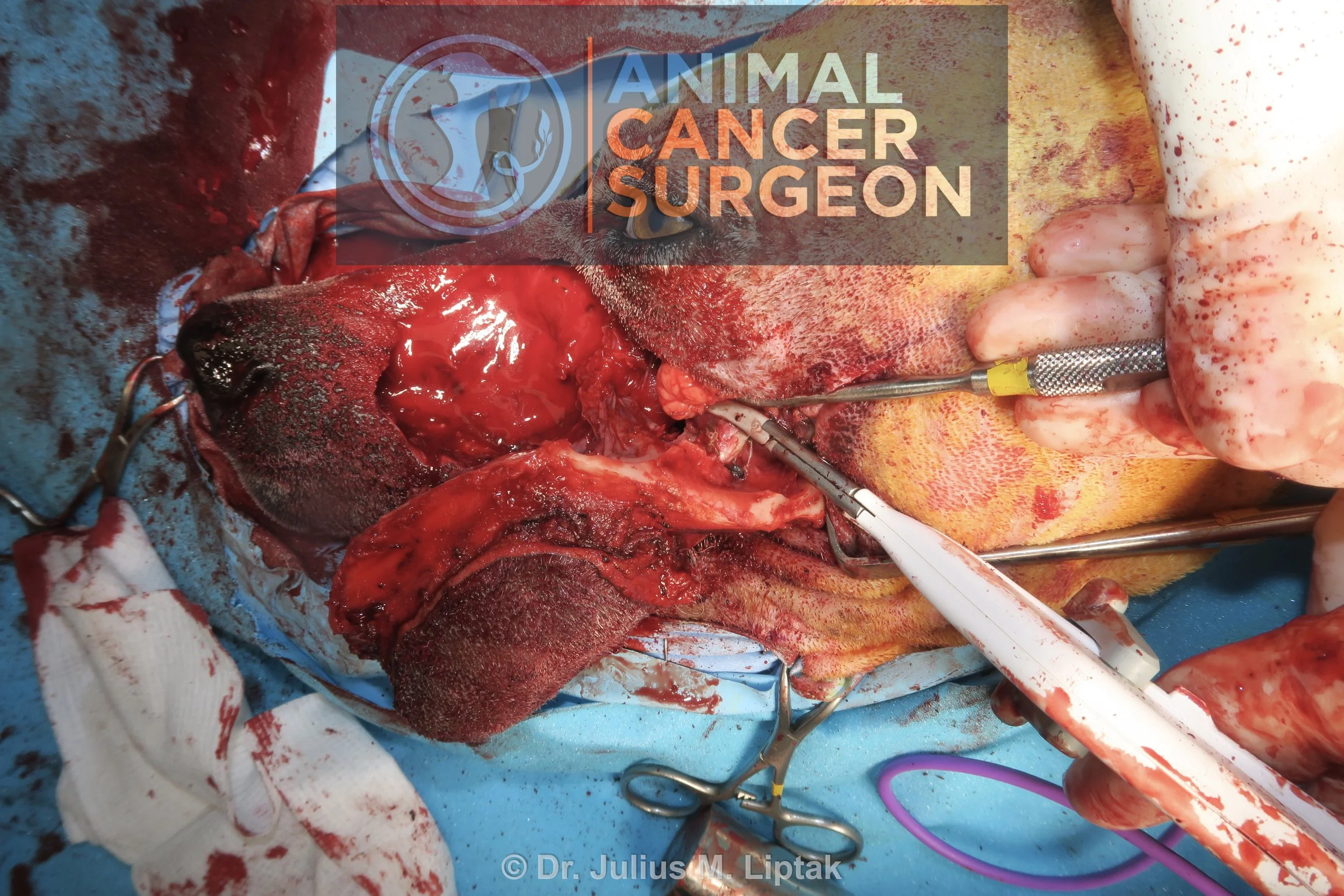
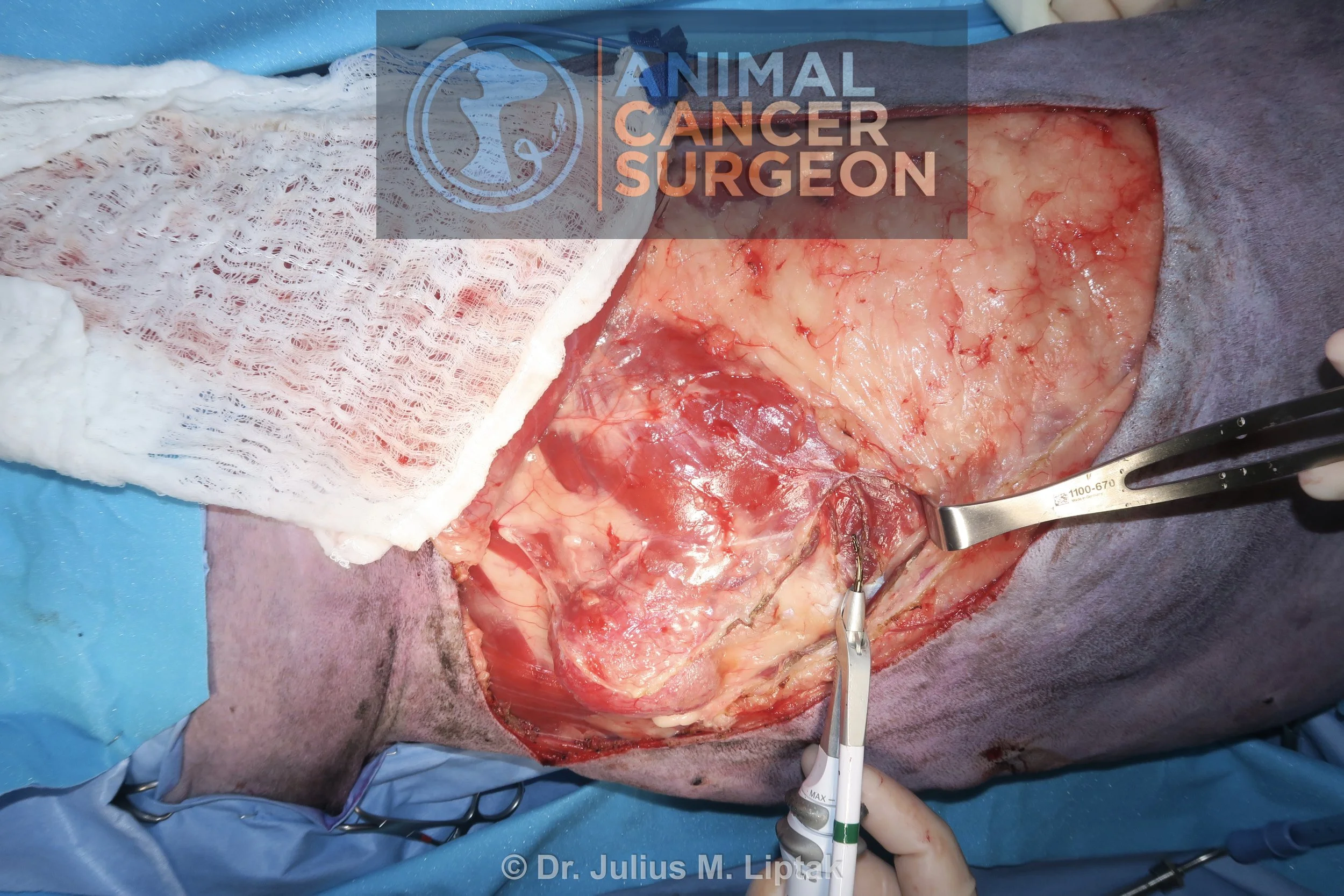
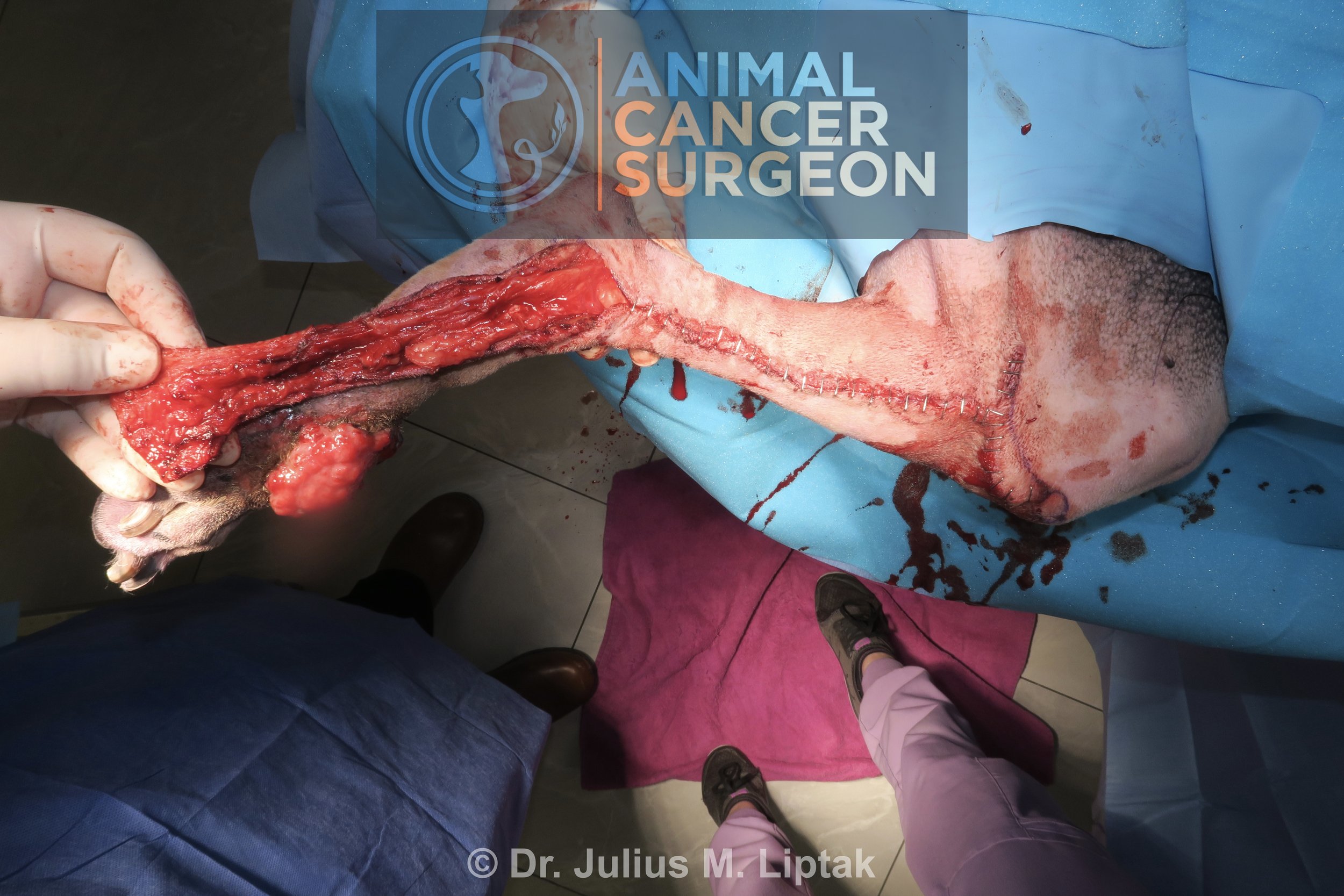
After much debate about positioning, she was positioned in dorsal recumbency. The standard intraoral approach was made for a mandibulectomy. A left commissurotomy was done to assess the caudal extent of the tumor. Unfortunately, her tumor extended to within millimetres of the caudal aspect of the vertical ramus. As a result, reconstruction was not possible and we had to perform a radical mandibulectomy instead. From this approach, her temporomandibular joint was disarticulated, an osteotomy of the right mid-mandible was performed with a sagittal saw (1 cm caudal to the caudal extent of the tumor on the right side), and then the mandibular segment was reflected laterally to seal and transect the mandibular alveolar artery and other soft tissues to complete the radical mandibulectomy. The mucosa was then closed, excessive skin on the ventral chin was resected, and the skin was then closed. An esophagostomy tube was placed because supplemental tube feeding is often required in the initial weeks following mandibulectomy in cats.
Outcome:
Grade II mandibular squamous cell carcinoma (SCC) with complete histologic (R0) excision, 3.3 mm histologic tumor-free margins on the lingual aspect, 2.6 mm ventrally, and caudal margins of 10 mm on the left side and 20 mm on the right side.
Died 6 days postoperatively of unknown causes in her sleep. She had no preceding signs of illness. Unfortunately for this owner, this cat was one of five in their household, two others of which died of respiratory-related illnesses in the same week as this cat with the other two being hospitalized with respiratory disease but later recovering.
Video link: https://lnkd.in/dWwetQMH
Notes:
While I am not sure if it would have made a difference for this owner, this cat was diagnosed cytologically with an osteosarcoma preoperatively but a SCC on definitive histopathology. Mandibular osteosarcomas have a more benign biological behaviour in cats whereas SCCs are more aggressive locally, which would explain the rapid tumor growth in the 3 weeks between her CT scan and surgery.
Tumor growth during the design and manufacture process is a known challenge when using patient-specific implants for reconstructing osseous defects following tumor resection. In one study of dogs treated with limb-sparing surgery using patient-specific implants, radiation therapy and intravenous chemotherapy were ineffective in limiting tumor growth during the period required for design and manufacture of the implant, with only regional intra-arterial chemotherapy being effective. Other options include modifying the implant design to account for estimated tumor growth (which I did in this case) or staging the resection and reconstruction so that the tumor is resected and then a CT is done immediately postoperatively and the defect is reconstructed after the implant has been designed, manufactured, and delivered. This latter option is acceptable for mandibular reconstructions but not for surgeries like limb salvage.
Despite the aggressiveness of this surgery, cats can do well following radical mandibuelctomy. In one study of eight cats treated with radical mandibulectomy, th mean survival time was 712 days and six of these cats returned to voluntary eating.
Tags: #SCC #FOSCC #mandibulectomy #patientspecifcimplant #PEKK